Oregano and Monolaurin as Antimicrobials-Study by Georgetown University
Effects of Essential Oils and Monolaurin on Staphylococcus aureus: In Vitro and In  Vivo Studies
Vivo Studies
Oregano and Monolaurin as Antimicrobials
Click on link below
Oregano and Monolaurin as Antimicrobials-Study by Georgetown University
Effects of Essential Oils and Monolaurin on Staphylococcus aureus: In Vitro and In  Vivo Studies
Vivo Studies
Oregano and Monolaurin as Antimicrobials
Click on link below
05 JUNE 2012
A recent publication in the prestigious Journal of Gastroenterology and Hepatology cites the effectiveness of acupuncture for the treatment of gastroesophageal reflux disease (GERD). Acupuncture was shown to be more effective in reducing regurgitation and heartburn than doubling medication  Acupuncture & GERDlevels for patients suffering from cases of refractory GERD. Dr. Ronnie Fass, MD of the University of Arizona in Tuscon reported that refractory GERD affects up to approximately one-third of patients who take PPIs (proton pump inhibitors). PPIs are pharmaceuticals that inhibit gastric acid production and include brand names such as Prilosec, Lomac, Prevacid, Nexium, andProtonix. Regarding the acupuncture research cited in the publication, Dr. Fass notes that, “This is the first study to suggest that alternative approaches for treating visceral pain may have a role in GERD patients with persistent heartburn despite PPI therapy.” Dr. Fass reported that for the approximately one-third of patients taking PPIs who continue to suffer from GERD, “When compared to doubling the PPI dose (standard of care), adding acupuncture was significantly better in controlling regurgitation and daytime as well as night-time heartburn.”
Acupuncture & GERDlevels for patients suffering from cases of refractory GERD. Dr. Ronnie Fass, MD of the University of Arizona in Tuscon reported that refractory GERD affects up to approximately one-third of patients who take PPIs (proton pump inhibitors). PPIs are pharmaceuticals that inhibit gastric acid production and include brand names such as Prilosec, Lomac, Prevacid, Nexium, andProtonix. Regarding the acupuncture research cited in the publication, Dr. Fass notes that, “This is the first study to suggest that alternative approaches for treating visceral pain may have a role in GERD patients with persistent heartburn despite PPI therapy.” Dr. Fass reported that for the approximately one-third of patients taking PPIs who continue to suffer from GERD, “When compared to doubling the PPI dose (standard of care), adding acupuncture was significantly better in controlling regurgitation and daytime as well as night-time heartburn.”
Reference:
Fass, R. (2012), Therapeutic options for refractory gastroesophageal reflux disease. Journal of Gastroenterology and Hepatology, 27: 3–7. doi: 10.1111/j.1440-1746.2012.07064.x
07 JUNE 2012
New research concludes that acupuncture combined with moxibustion successfully alleviates herpes zoster neuralgia, nerve pain due to shingles. A total 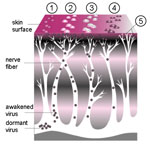 Acupuncture for Shinglesof 37 cases were divided into two groups. Group 1, the medication group of 19 cases, received ibuprofen, vitamin B1 and vitamin E. Group 2, the treatment group of 18 cases, received acupuncture and herbal moxa roll heat stimulation. The herbal moxa roll consisted of corydalis tuber (Yan Hu Suo), astragali radix (Huang Qi), myrrh (Mo Yao) and other related herbal ingredients. Moxibustion was applied once a day for 7 days to Jiaji (EX-B-2) and Ahshi acupuncture points until local skin flushing was obtained. Acupuncture was applied to the same acupoints, Ahshi and Jiaji points, at a rate of once per day for 7 days. Acupuncture technique was applied using electroacupuncture at 100 Hz for 10 minutes followed by 2 Hz stimulation for an additional 30 minutes.
Acupuncture for Shinglesof 37 cases were divided into two groups. Group 1, the medication group of 19 cases, received ibuprofen, vitamin B1 and vitamin E. Group 2, the treatment group of 18 cases, received acupuncture and herbal moxa roll heat stimulation. The herbal moxa roll consisted of corydalis tuber (Yan Hu Suo), astragali radix (Huang Qi), myrrh (Mo Yao) and other related herbal ingredients. Moxibustion was applied once a day for 7 days to Jiaji (EX-B-2) and Ahshi acupuncture points until local skin flushing was obtained. Acupuncture was applied to the same acupoints, Ahshi and Jiaji points, at a rate of once per day for 7 days. Acupuncture technique was applied using electroacupuncture at 100 Hz for 10 minutes followed by 2 Hz stimulation for an additional 30 minutes.
Following the 7 day session, one patient in the medication group was diagnosed as cured while 5 patients in the acupuncture combined with moxibustion group were diagnosed as cured. Significant improvement was diagnosed in 13 patients in the medication group and 12 patients in the acupuncture combined with moxibustion group. No progress was reported in 5 patients in the medication group while only one patient in the acupuncture-moxibustion group did not respond to therapy. The researchers discovered that the therapeutic effect achieved in the acupuncture with moxibustion group “was significantly superior to that of the medication group.” The researchers concluded that electroacupuncture with moxibustion “is effective in relieving neuralgia in HZ (herpes zoster) patients.”
Reference:
Zhen Ci Yan Jiu. 2012 Feb;37(1):64-6. Analysis on therapeutic effect of variable-frequency electroacupuncture combined with herbal-moxa moxibustion for post-zoster neuralgia. Wang CY, Fang JQ. The Third Affiliated Hospital of Zhejiang University of Chinese Medicine, Hangzhou. China.
By Brenda Duran, Senior Associate Editor

For people living with Parkinson’s disease, the future is full of obstacles and uncertainty.
This is the sole reason the second most prevalent neuro-degenerative disease that affects about 1 million people in the U.S., and 5 million worldwide has researchers constantly on the hunt for not only a cure, but also a way to improve the quality of life for patients.
By the year 2013, a current research study involving acupuncture is hoping to find answers for Parkinson’s disease patients living with one of the most debilitating side effects – fatigue.![]()
The research study funded by the Michael J. Fox Foundation for Parkinson’s Research is currently determining whether alternative Eastern medicine, specifically acupuncture, can help alleviate symptoms of severe fatigue in those living with Parkinson’s.
The foundation, which was established in 2000 by actor Michael J. Fox, is the largest funder of Parkinson’s research in the world. The organization has funded over $270 million in targeted Parkinson’s research to date including the latest study on acupuncture.
Dr. Benzi Kluger, assistant professor of neurology and psychiatry at the University of Colorado Hospital has been leading the study, which began in November 2010. The study is being conducted as a double-blind study to find whether acupuncture has a significant effect on Parkinson’s patients living with fatigue in their daily lives.
“Western medicine does not have good treatment for fatigue,” said Kluger. “Fatigue for patients with Parkinson’s is really different, it doesn’t improve with rest and is very disabling.”
 Fatigue affects approximately half of all Parkinson’s disease patients. Many of them do not get relief from medication and research has now focused on ancient Eastern medicine such as acupuncture to find answers, said Kluger.
Fatigue affects approximately half of all Parkinson’s disease patients. Many of them do not get relief from medication and research has now focused on ancient Eastern medicine such as acupuncture to find answers, said Kluger.
“We wanted to see if we can come up with alternative strategies that can also later help people with other neurological disorders in the future,” said Kluger.
Kluger approached the Parkinson’s foundation with his study because he said he was interested in non-motor systems in Parkinson’s patients. Non-motor symptoms are the most common symptoms that develop first in patients and one of them is fatigue.
Jamie Eberling, associate director of research programs at the Michael J. Fox Foundation for Parkinson’s Research said Kluger’s study was chosen based on its merits and because it was something of interest to their donor base.
“We are always interested in different types of approaches,” said Eberling. “We are always open to new things, we wish we could see more of these types of studies being presented.”
The foundation in the past has funded studies on exercise and even singing for speech problems as well as dancing for motor impairment in Parkinson’s disease patients. They review 800 grant proposals a year and are currently supporting more than 300 research projects in industry, academia and government.
Kluger’s acupuncture study has a total of 22 patients participating right now. The goal is to have 90-100 patients by the study’s end date in 2013.
Patients who joined the study initially came in for a screening visit and filled out a questionnaire about fatigue and their beliefs about acupuncture and alternative medicine. Once people were screened into the study, they were randomized with twice weekly sham or real acupuncture.
Patients in the study are blindfolded while they are receiving acupuncture treatment and Kluger said he doesn’t know which patients are receiving acupuncture treatment and which patients are receiving placebo.
Three acupuncturists have been working on the study subjects placing needles in acupuncture points on the patient’s face and back. For patients who are in the placebo group, the acupuncturists may place non-penetrating needles in spots that aren’t typical acupuncture spots.
Kluger said in the spring, his team is going to try to shell out a paper on the sham acupuncture after spending a lot of time learning how to remove the sham needles to create a really good placebo procedure.
So far, Kluger said he has seen dramatic improvement in fatigue in some of the study subjects. “People have gone back to doing activities that they haven’t done in years,” he said. Since the statistical data is not yet completed, Kluger said he wouldn’t know which group has benefitted the most.
Kluger noted that a large majority of Parkinson’s disease patients already use a form of alternative medicine – acupuncture, massage, herbs and chiropractic care, but until now, there weren’t many evidence-based studies to determine whether acupuncture is effective for symptoms such as fatigue.
The neuro-degenerative disease affects between 1 percent and 2 percent of people over the age of 65. Those diagnosed with the disease will lose neurons in specific parts of the brain, affecting muscle movement and control over time.
Kluger said if he finds that acupuncture can be used as an alternative form of medicine to alleviate the symptoms of severe fatigue, it might help insurance companies extend their coverage of the treatment.
“We will also be able to see if acupuncture would be effective for people with other diseases like cancer and MS (Multiple Sclerosis),” Kluger said.
Focusing most of his medical career in Western medicine, Kluger said he has really enjoyed doing research on Eastern medicine and finding out about the potential it has to heal people.
“For me it has been a wonderful opportunity to work with acupuncturists to really start to delve into acupuncture. One of my goals is to come out of it with an open mind,” he said. “It’s been really fun to explore alternative ways to help these patients. We are hopeful.”
If you would like to know more about the study contact etta.abaca@ucdenver.edu or call 303-724-2193.
Asthma affects millions of adults and children in the United States. Its increasing prevalence, the absence of curative treatments, and concerns about side effects from long-term use of asthma drugs have prompted interest in complementary and alternative therapies such as traditional Chinese medicine (TCM) herbs.
In a recent article, NCCAM-supported scientists from the Mount Sinai School of Medicine reviewed research  evidence on TCM herbs for asthma, focusing on studies reported since 2005:
evidence on TCM herbs for asthma, focusing on studies reported since 2005:
The authors noted that clinical trials are under way for ASHMI. They also summarize research on a TCM formula being developed to combat peanut allergy.


Stephen M. Stahl, MD, PhD
CNS Spectr. 2007;12(10):739-7 Faculty Affiliation and DisclosuresDr. Stahl is adjunct professor of psychiatry in the Department of Psychiatry at the University of California-San Diego in La Jolla.Disclosures: Dr. Stahl receives grant/research support from AstraZeneca, Biovail, Bristol-Myers Squibb, Cephalon, Cyberonics, Eli Lilly, Forest, GlaxoSmithKline, Janssen, Neurocrine Bioscience, Organon, Pfizer, Sepracor, Shire, Somaxon, and Wyeth; is a consultant to Acadia, Amylin, Asahi, AstraZeneca, Biolaunch, Biovail, Boehringer-Ingelheim, Bristol-Myers Squibb, Cephalon, CSC Pharma, Cyberonics, Cypress Bioscience, Eli Lilly, Epix, Fabre Kramer, Forest, GlaxoSmithKline, Jazz, Neurocrine Bioscience, Neuromolecular, Neuronetics, Nova Del Pharma, Novartis, Organon, Otsuka, PamLab, Pfizer, Pierre Fabre, Sanofi Synthelabo, Schering Plough, Sepracor, Shire, Solvay, Somaxon, Takeda, Tetragenix, and Wyeth; and is on the speaker’s bureau of Pfizer.Email Dr. Stahl: vj@mblcommunications.com.
Activated Folate-MTHF from Thorne Research Available
Denise Lane-Acupuncturist
New Trend in Psychopharmacology
Folate deficiency may increase the risk of depression and reduce the action of antidepressants. Individuals with an inherited polymorphism that reduces the efficiency of folate formation may be at high risk for folate deficiency and for major depression. Antidepressant effects have been reported when antidepressants are augmented with folic acid, folinic acid, or the centrally active L-methylfolate (known formally as (6(S)-5-methyltetrahydrofolate [MTHF]), particularly in depressed patients with folate deficiency whose major depressive episodes have failed to respond to antidepressants. The putative mechanism of action of MTHF as an augmenting agent to antidepressants is that it acts as a trimonoamine modulator (TMM), enhancing the synthesis of the three monoamines: dopamine (DA), norepinephrine (NE), and serotonin (5-HT), resulting in a boost to the efficacy of antidepressants.
Folate and Depression
A substantial body of literature suggests that depression is associated with folate deficiency,1-31 and that patients with folate deficiency either experience a later onset of action,2,19 lesser improvement,4,8,9,13 a more severe depressive episode,8,19-21 or higher chances of relapse14 when taking antidepressants. The link between folate and depression is supported by observations that a common genetic variant of an enzyme that reduces one’s ability to convert folate to its centrally active metabolite, MTHF, specifically, the C677T variant of the enzyme methylene tetrahydrofolate reductase, is more common in patients with depression.15,26-28 In this article and in the figures, the centrally active metabolite of folate will be referred to either as L-methylfolate or as MTHF.

The formation of MTHF from foods containing dihydrofolate or enriched with synthetic folic acid is shown in Figure 1. The enzyme methylene tetrahydrofolate reductase forms this centrally active metabolite, MTHF, in the final step of this process (Figure 1). The link between folate and depression is also supported by numerous studies suggesting that folic acid,16,17 folinic acid,31 or MTHF18,32-35 either have antidepressant action or enhance the therapeutic benefits of antidepressants or lithium.
How Does L-methylfolate Act as an Antidepressant?
Antidepressants boost the actions of one or more of the three monoamines: DA, NE, and/or 5-HT. MTHF acts as an important regulator of a critical co-factor for trimonoamine neurotransmitter synthesis. This co-factor is known as tetrahydrobiopterin (BH4) (Figure 2A).36-48 By boosting trimonoamine neurotransmitter synthesis via enhancement of BH4, MTHF presumably is able to augment the antidepressant actions of known antidepressants.
Because BH4 is a critical enzyme co-factor, there are several mechanisms that lead to its formation (Figure 2B).36-48 BH4 can be formed from de novo synthesis, from guanosine triphosphate, or recycled via the enzyme dihydropteridine reductase (Figure 2B).38,39,44 BH4 formation that is linked to folate metabolism includes recycling either from the actions of methylene tetrahydrofolate reductase (mentioned above)44,45 or from the actions of dihydrofolate reductase (Figure 2B).37,43
The trimonoamine synthetic enzymes that require BH4 as a co-factor are tryptophan hydroxylase, the rate-limiting enzyme for 5-HT synthesis and tyrosine hydroxylase, the rate-limiting enzyme for DA and NE synthesis (Figure 3).36,39,42 MTHF is thus considered to be a TMM due to its role as an indirect regulator of trimonoamine neurotransmitter synthesis and monoamine concentrations.48
As previously mentioned, numerous studies suggest that low plasma, red blood cell, and/or cerebrospinal fluid levels of MTHF folate precursors (Figure 1) may be associated with depression in some patients (Figure 4A).1-30 Since MTHF indirectly regulates monoamine levels (Figures 2 and 3),36-48 low central nervous system levels of MTHF could lead to reduced activity of trimonoaminergic neurotransmitter-synthesizing enzymes, causing monoamine deficiency (Figure 4A), consistent with the monoamine hypothesis of depression.46-48
Studies16-35 have now shown that administration of folate, MTHF, or another folate derivative known as folinic acid (Leucovorin), can augment the therapeutic efficacy of antidepressants in patients with major depressive disorder who fail to respond adequately to their antidepressant, and who may or may not have measurable folate deficiency. Current research thus suggests that MTHF may be indicated for depressed patients with low plasma, red blood cell, and/or cerebrospinal fluid folate levels, and who have not responded adequately to antidepressants (Figure 4B).16-35 Theoretically, many patients with inadequate responses to a monoamine-enhancing antidepressant, even if there is no folate deficiency, could benefit from MTHF treatment that elevates their BH4 levels (Figure 1), if it led to enhancement of their trimonoamine neurotransmitter synthesis (Figure 3; also compare Figures 4A and 4B).36-48
Why L-methylfolate Rather Than Folic Acid for Depression?
Folate is one of the 13 essential vitamins. Dihydrofolate, a mixture of polyglutamates (ie, a number of glutamatic acid entities) is the form of folate obtained from dietary intake of green vegetables, yeast, liver, kidney, and egg yolk. Folic acid is the synthetic form of folate contained in over-the-counter vitamin supplements (usually mixed with several other vitamins and nutrients and present in low doses). Folic acid is also the synthetic form of folate contained in prescriptions written by a licensed practitioner in higher doses for medical use.
Dihydrofolate and folic acid are converted to monoglutamate entites by the enzyme alpha-L-glutamyl transferase in the intestinal wall as they are absorbed.47 Once absorbed, monoglutamate entities are converted to MTHF, the form of folate that passes into the brain and is utilized by trimonoamine neurons to facilitate neurotransmitter synthesis (Figures 1 and 4B). Normally, ingesting folate from dihydrofolate in the diet or from folic acid in synthetic supplements will result in adequate delivery of MTHF levels to the brain, especially in those individuals with the more efficient genotype (C677C) producing up to 100% of the enzyme methylene tetrahydrofolate reductase and who do not have depression.
However, robust levels of MTHF in the brain, which may be necessary to maximize the chances of boosting trimonoamine neurotransmitter synthesis (Figures 2–4), are more likely attained after administration of MTHF rather than folic acid (Figure 4B). Thus, administration of MTHF may have significant advantages over administration of folic acid as a TMM to augment antidepressants in depressed patients who do not respond adequately to their antidepressant treatment. Such patients may or may not be folate deficient, may or may not have the inefficient form of the genotype (C677T, T677T) producing 35% to 71% of the MTHF enzyme, and may or may not be taking various anticonvulsant mood stabilizers that interfere with folic acid absorption or MTHF formation, such as lamotrigine, carbamazepine, and others (Figure 4B). Further research is needed to identify those depressed patients most likely to respond to MTHF augmentation, including studies of both unipolar and bipolar depression.
In terms of what is known about treatment with folic acid versus MTHF, it may take as much as 7 mg of oral folic acid to generate the same plasma levels of MTHF as giving 1 mg of oral MTHF.49 How much folic acid is this? The recommended daily allowance of folic acid from food or dietary supplements is 0.4 mg (0.8 mg for pregnant women); over-the-counter multivitamin supplements typically provide between 0.25 and 1 mg of folic acid; normal “prescription strength” folic acid is 1 mg pure folic acid; high-dose prescription folic acid for treating pregnant women to reduce the risk of neural tube defects is between 4 mg and 5 mg. By comparison, the lowest dose of MTHF studied in depression to augment antidepressant treatment is 7.5 mg, roughly equivalent to 52 mg of folic acid.32 Although high doses of folic acid can be administered orally, the precursors of MTHF may compete with MTHF for entry into brain by binding to folate transport receptors, limiting the amount of MTHF that can enter the brain (Figure 4B).50-52 Thus, high doses of MTHF are likely to provide substantially more active MTHF moiety to the brain than high doses of folic acid. The exact dose of MTHF to treat depression is not fully determined, but since MTHF works indirectly to boost monoamine synthesis, high doses are likely to be necessary to optimize this action.
Additionally, high doses of MTHF may be more appropriate than high doses of folic acid because MTHF is less likely to mask a vitamin B12 deficiency.53-55 That is, when folic acid is administered, it can be metabolized and utilized for DNA biosynthesis even in vitamin B12 deficient cells, thus masking the anemia from a vitamin B12 deficiency. B12 deficiency decreases the methyl donor S-adenosyl-methionine (SAMe), which activates the enzyme MTHF reductase and this traps MTHF away from DNA synthesis, making it unlikely that the administration of MTHF will mask an anemia.53-56
What is a Medical Food?
MTHF is marketed in the United States as a “medical food” also called Deplin, which contains 7.5 mg L-methylfolate and is available by prescription only. According to the Food and Drug Administration, a medical food is different both from a drug and from a food, and is defined as a food that is formulated to be consumed orally
“…under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.”57
Medical foods are required when dietary management cannot achieve the specific nutrient requirements. Treatment with MTHF seems to be safe, apparently has few if any side effects, and is generally less expensive than augmenting with a second antidepressant. Further research is necessary to determine the exact priority this approach should be given in treatment algorithms for major depression.
S-adenosyl-methionine, L-methylfolate, and Methylation
MTHF may have additional actions on monoamine neurotransmitter metabolism through another mechanism, namely, its well-known ability to regulate methylation reactions (Figure 5).37 Another agent possibly useful for augmenting antidepressants in patients with inadequate responses is SAMe, which shares with MTHF the ability to regulate methylation (Figure 5).58,59 Both MTHF and SAMe may therefore impact the regulation of various critical  components of monoamine neurotransmitter activity not only by indirect modulation of neurotransmitter synthesis by promoting the synthesis of BH4 enzymatic cofactor, but also by modulating catabolic enzymes, monoamine transporters, and neurotransmitter receptors via methylation and its downstream effects (Figure 5).60-65 These complex mechanisms are under active investigation to determine how the natural products and putative TMMs, MTHF and SAMe, may contribute to the treatment of depression.
components of monoamine neurotransmitter activity not only by indirect modulation of neurotransmitter synthesis by promoting the synthesis of BH4 enzymatic cofactor, but also by modulating catabolic enzymes, monoamine transporters, and neurotransmitter receptors via methylation and its downstream effects (Figure 5).60-65 These complex mechanisms are under active investigation to determine how the natural products and putative TMMs, MTHF and SAMe, may contribute to the treatment of depression.
Conclusion
L-methylfolate, also known as MTHF (methyltetrahydrofolate), acts as a trimonoamine modulator to boost the synthesis of the three monoamines: DA, NE, and 5-HT. This action may provide antidepressant efficacy when L-methylfolate is given as an augmenting agent to depressed patients unresponsive to traditional antidepressants. L-methylfolate may be especially useful in depressed patients who have the genotype coding for an enzyme that causes inefficient synthesis of L-methylfolate, and for those individuals who are folate deficient, including patients whose folate deficiency is secondary to the administration of various anticonvulsant mood stabilizers.
References
1. Coppen A, Bolander-Gouaille C. Treatment of depression: time to consider folic acid and vitamin B12. J Psychopharmacol. 2005;19:59-65.
2. Papakostas GI, Petersen T, Lebowitz BD, et al. The relationship between serum folate, vitamin B12, and homocysteine levels in major depressive disorder and the timing of improvement with fluoxetine. Int J Neuropsychopharmacol. 2005;8:523-528.
3. Tolmunen T, Voutilainen S, Hintikka J, et al. Dietary folate and depressive symptoms are associated in middle-aged Finnish men. J Nutr. 2003;133:3233-3236.
4. Alpert M, Silva RR, Pouget ER. Prediction of treatment response in geriatric depression from baseline folate level: interaction with an SSRI or a tricyclic antidepressant. J Clin Psychopharmacol. 2003;23:309-313.
5. Morris MS, Fava M, Jacques PF, Selhub J, Rosenberg IH. Depression and folate status in the US Population. Psychother Psychosom. 2003;72:80-87.
6. Bottiglieri T, Laundy M, Crellin R, Toone BK, Carney MW, Reynolds EH. Homocysteine, folate, methylation, and monoamine metabolism in depression. J Neurol Neurosurg Psychiatry. 2000;69:228-232.
7. Alpert JE, Fava M. Nutrition and depression: the role of folate. Nutr Rev. 1997;55:145-149.
8. Fava M, Borus JS, Alpert JE, Nierenberg AA, Rosenbaum JF, Bottiglieri T. Folate, vitamin B12, and homocysteine in major depressive disorder. Am J Psychiatry. 1997;154:426-428.
9. Wesson VA, Levitt JA, Joffe RT. Change in folate status with antidepressant treatment. Psychiatry Res. 1994;53:313-322.
10. Coppen A, Swade C, Jones SA, Armstrong RA, Blair JA, Leeming RJ. Depression and tetrahydrobiopterin: the folate connection. J Affect Disord. 1989;16:103-107.
11. Abou-Saleh MT, Coppen A. Serum and red blood cell folate in depression. Acta Psychiatr Scand. 1989;80:78-82.
12. Abou-Saleh MT, Coppen A. The biology of folate in depression: implications for nutritional hypotheses of the psychoses. J Psychiatr Res. 1986;20:91-101.
13. Papakostas GI, Petersen T, Mischoulon D, et al. Serum folate, vitamin B12, and homocysteine in major depressive disorder, Part 1: predictors of clinical response in fluoxetine-resistant depression. J Clin Psychiatry. 2004;65:1090-1095.
14. Papakostas GI, Petersen T, Mischoulon D, et al. Serum folate, vitamin B12, and homocysteine in major depressive disorder, Part 2: predictors of relapse during the continuation phase of pharmacotherapy. J Clin Psychiatry. 2004;65:1096-1098.
15. Gilbody S, Lewis S, Lightfoot T. Methylene tetrahydro folate reductase (MTHFR) genetic polymorphisms and psychiatric disorders: a HuGE review. Am J Epidemiol. 2006;165:1-13.
16. Coppen A, Bailey J. Enhancement of the antidepressant action of fluoxetine by folic acid: a randomised, placebo controlled trial. J Affect Disord. 2000;60:121-130.
17. Coppen A, Chaudhry C, Swade C. Folic acid enhances lithium prophylaxis. J Affect Disord. 1986;10:9-13.
18. Passeri M, Cucinotta D, Abate G, et al. Oral 5’-methyltetrahydrofolic acid in senile organic mental disorders with depression: results of a double-blind multicenter study. Aging (Milano). 1993;5:63-71.
19. Carney MW, Chary TK, Laundy M. Red cell folate concentrations in psychiatric patients. J Affect Disord. 1990;19:207-213.
20. Reynolds EH, Preece JM, Bailey J, Coppen A. Folate deficiency in depressive illness. Br J Psychiatry. 1970;117:287-292.
21. Lerner V, Kanevsky M, Dwolatzky T, Rouach T, Kamin R, Miodownik C. Vitamin B12 and folate serum levels in newly admitted psychiatric patients. Clin Nutr. 2006;25:60-67.
22. Sachdev PS, Parslow RA, Lux O, et al. Relationship of homocysteine, folic acid and vitamin B12 with depression in a middle-aged community sample. Psychol Med. 2005;35:529-538.
23. Levitt AJ, Joffe RT. Folate, B12, and life course of depressive illness. Biol Psychiatry. 1989;25:867-872.
24. Wesson VA, Levitt AJ, Joffe RT. Change in folate status with antidepressant treatment. Psychiatry Res. 1994;53:313-322.
25. Wilkinson A, Anderson D, Abou-Saleh M, et al. 5-Methyltetrahydrofolate level in the serum of depressed subjects and its relationship to the outcome of ECT. J Affect Disord. 1994;32:163-168.
26. Kelly CB, McDonnell AP, Johnston TG, et al. The MTHFR C677T polymorphism is associated with depressive episodes in patients from Northern Ireland. J Psychopharmacol. 2004;18:567-571.
27. Lewis SJ, Lawlor DA, Davey Smith G, et al. The thermolabile variant of MTHFR is associated with depression in the British Women’s Heart and Health Study and a meta-analysis. Mol Psychiatry. 2006;11:352-360.
28. Arinami T, Yamada N, Yamakawa-Kobayashi K, et al. Methylenetetrahydrofolate reductase variant and schizophrenia/depression. Am J Med Genet. 1997;74:526-528.
29. Gilbody S, Lightfoot T, Shelton T. Is low folate a risk factor for depression? A meta-analysis and exploration of heterogeneity. J Epidemiol Community Health. 2007;61:631-637.
30. Blair JA, Barford PA, Morar C, et al. Tetrahydrobiopterin metabolism in depression. Lancet. 1984;2:163.
31. Alpert JE, Mischoulon D, Rubenstein GE, Bottonari K, Nierenberg AA, Fava M. Folinic acid (Leucovorin) as an adjunctive treatment for SSRI-refractory depression. Ann Clin Psychiatry. 2002;14:33-38.
32. Guaraldi GP, Fava M, Mazzi F, la Greca P. An open trial of methyltetrahydrofolate in elderly depressed patients. Ann Clin Psychiatry. 1993;5:101-105.
33. Godfrey PS, Toone BK, Carney MW, et al. Enhancement of recovery from psychiatric illness by methylfolate. Lancet. 1990;336:392-395.
34. Reynolds EH, Crellin R, Bottiglieri T, Laundy M, Toone BK, Carney M. Methylfolate as monotherapy in depression: a pilot randomized controlled trial. Abstract presented at: the Annual Meeting of the Royal College of Psychiatrists. July 24-27, 1992; Edinburgh, UK.
35. Di Palma C, Urani R, Agricola R, Giorgetti V, Dalla Verde G. Is Methylfolate effective in relieving major depression in chronic alcoholics? A hypothesis of treatment. Curr Ther Res. 1994;55:559-568.
36. Meller E, Friedhoff AJ. 5-methyltetrahydrofolate and metabolism of biogenic amines; In: Botez MI, Reynolds EH, eds. Folic Acid in Neurology, Psychiatry and Internal Medicine. New York, NY: Raven Press; 1979:157-164.
37. Bottiglieri T, Hyland K, Laundry M, et al. Folate deficiency, biopterin and monoamine metabolism in depression. Psychol Med. 1992;22:871-876.
38. Ponzone A, Spada M, Ferraris S, Dianzani I, deSanctis L. Dihydropteridine reductase deficiency in man: from biology to treatment. Med Res Rev. 2004;24:127-150.
39. Goldstein DS, Hahn S-H, Holmes C, et al. Monoaminergic effects of folinic acid, l-dopa and 5-hydroxytryptophan in dihydropteridine reductase deficiency. J Neurochem. 1995;64:2810-2813.
40. Lucock MD, Green M, Levene MI. Methylfolate modulates potassium evoked neuro-secretion: evidence for a role at the pteridine cofactor level of tyrosine 3-hydroxylase. Neurochem Res. 1995;20:727-736.
41. Niederwieser A. Inborn errors of Pterin metabolism. In: Botez MI, Reynolds EH, eds. Folic Acid in Neurology, Psychiatry and Internal Medicine. New York, NY: Raven Press; 1979:349-384.
42. Turner AJ. The relationship between brain folate and monoamine metabolism. In: Botez MI, Reynolds EH, eds. Folic Acid in Neurology, Psychiatry and Internal Medicine. New York, NY: Raven Press; 1979:165-177.
43. Hamon CGB, Blair JA, Barford PA. The effect of tetrahydrofolate on tetrahydrobipterin metabolism. J Ment Defic Res. 1986;30:179-183.
44. Matthews RG, Kaufman S. Characterization of the dihydropterin reductase activity of pig liver methylenetetrahydrofolate reductase. J Biol Chem. 1980;255:6014-6017.
45. Vanoni MA, Ballou DP, Matthews RG. Methylenetetrahydrofolate reductase. Steady state and rapid reaction studies on the NADPH-methylenetetrahydrofolate, NADPH-menadione, and methyltetrahydrofolate-menadione oxidoreductase activities of the enzyme. J Biol Chem. 1983;258:11510-11514.
46. Farrar G, Blair JA. Pterins in depression: a modified monoamine hypothesis. In: Copeland JR, Abou-Saleh MT, Blazer DG, eds. Principles and Practice of Geriatric Psychiatry. Hoboken, NJ: John Wiley and Sons; 1994:543-546.
47. Paul RT, McDonnell AP, Kelly CB. Folic acid: neurochemistry, metabolism and relationship to depression. Hum Psychopharmacol. 2004;19:477-488.
48. Stahl SM. Essential Psychopharmacology. 3rd ed. New York, NY: Cambridge University Press; In press.
49. Willems FF, Boers GH, Blom HJ, Aengevaeren WR, Verheugt FW. Pharmacokinetic study on the utilisation of 5-methyltetrahydrofolate and folic acid in patients with coronary artery disease. Br J Pharmacol. 2004;141:825-830.
50. Smith I, Hyland K, Kendall B. Clinical role of pteridine therapy in tetrahydrobiopterin deficiency. J Inherit Metab Dis. 1985;8(suppl 1):39-45.
51. Wu D, Pardridge WM. Blood-brain barrier transport of reduced folic acid. Pharm Res.1999;16:415-419.
52. Spector R, Lorenzo AV. Folate transport in the central nervous system. Am J Physiol. 1975;229:777-782.
53. Scott JM, Weir DG. The methyl folate trap. A physiological response in man to prevent methyl group deficiency in kwashiorkor (methionine deficiency) and an explanation for folic-acid induced exacerbation of subacute combined degeneration in pernicious anaemia. Lancet. 1981;2:337-340.
54. Kelly P, McPartlin J, Goggins M, Weir D, Scott JM. Unmetabolized folic acid in serum: acute studies in subjects consuming fortified food and supplements. Am J Clin Nutr. 1997;65:1790-1795.
55. Morris MS, Jacques PF, Rosenberg IH, Selhub J. Folate and vitamin B-12 status in relation to anemia, macrocytosis, and cognitive impairment in older Americans in the age of folic acid fortification. Am J Clin Nutr. 2007;85:193-200.
56. Akoglu B, Schrott M, Bolouri H, et al. The folic acid metabolite L-5-methyltetrahydrofolate effectively reduces total serum homocysteine level in orthotopic liver transplant recipients: a double-blind placebo-controlled study. Eur J Clin Nutr. In press.
57. Food and Drug Administration/Center for Food Safety and Applied Nutrition. Food Safety and Applied Nutrition, Medical Foods. Available at: http://www.cfsan.fda.gov/~dms/medfguid.html. Accessed September 13, 2007.
58. Mischoulon D, Fava M. Role of S-adenosyl-L-methionine in the treatment of depression: a review of the evidence. Am J Clin Nutr. 2002;76(suppl):1158S-1161S.
59. Bottiglieri T. S-Adenosl-L-methionine (SAMe): from the bench to the bedside – molecular basis of a pleiotrophic molecule. Am J Clin Nutr. 2002;76(suppl):1151S-1157S.
60. Vafai SB, Stock JB. Protein phosphatase 2A methylation: a link between elevated plasma homocysteine and Alzheimer’s disease. FEBS Lett. 2002;518:1-4.
61. Mann SP, Hill MW. Activation and inactivation of striatal tyrosine hydroxylase: the effects of pH, ATP, cyclic AMP, S-adenosylmethionine and S-adenosylhomocysteine. Biochem Pharmacol. 1983;32:3369-3374.
62. Curcio M, Catto E, Stramentinoli G, Algeri S. Effect of S-adenosyl-l-methionine on serotonin metabolism in rat brain. Prog Neuropsychopharmacol. 1978;2:65-71.
63. Ruck A, Kramer S, Metz J, Brennan MJ. Methyltetrahydrofolate is a potent and selective agonist for kainic acid receptors. Nature. 1980;287:852-853.
64. Bauman AL, Apparsundaram S, Ramamoorthy S, Wadzinski BE, Vaughan RA, Blakely RD. Cocaine and antidepressant-sensitive biogenic amine transporters exist in regulated complexes with protein phosphatase 2A. J Neurosci. 2000;20:7571-7578.
65. Ramamoorthy S, Gioivanetti E, Qian Y, Blakely RD. Phosphorylation and regulation of antidepressant-sensitive serotonin transporters. J
Novel Therapeutics for Depression: L-methylfolate as a Trimonoamine Modulator and Antidepressant-Augmenting Agent
Inflammation, Glutamate, and Glia in Depression: A Literature Review
Beyond the Dopamine Hypothesis to the NMDA Glutamate Receptor Hypofunction Hypothesis of Schizophrenia
Bipolar Depression: Best Practices for the Outpatient
Home | About Us | Contact Us | Our Mission | Journal CME | CME Enduring Materials
Clinical Supplements | Clinical Columns/News | Disease States | Advisory Board | Services & Online Store
Partner/Alliances | © 2012
Privacy Policy | Site Map | Web design and development by Spindustry Interactive
Author: Ladan Eshkevari, an assistant professor at Georgetown’s School of Nursing & Health Studies (NHS), part of GUMC.
 “It has long been thought that acupuncture can reduce stress, but this is the first study to show molecular proof of this benefit,” says Ladan Eshkevari, lead author of the study and assistant professor in the School of Nursing & Health Studies.
“It has long been thought that acupuncture can reduce stress, but this is the first study to show molecular proof of this benefit,” says Ladan Eshkevari, lead author of the study and assistant professor in the School of Nursing & Health Studies.DECEMBER 20, 2011 – ACUPUNCTURE SIGNIFICANTLY REDUCES LEVELS of a protein linked to chronic stress, according to a study with rats by researchers atGeorgetown University Medical Center (GUMC). The study may help explain the sense of well-being many people say they get from this ancient Chinese therapy. Published online in Experimental Biology and Medicine earlier this month, the researchers say that if their findings can be replicated in humans, acupuncture would become a proven therapy for stress.
“It has long been thought that acupuncture can reduce stress, but this is the first study to show molecular proof of this benefit,” says the study’s lead author, Ladan Eshkevari, an assistant professor at Georgetown’s School of Nursing & Health Studies (NHS), part of GUMC. Eshkevari, assistant director of the Nurse Anesthesia Program and a certified acupuncturist, says she conducted the study because many of the patients she treats with acupuncture report a “better overall sense of well-being – and they often remarked that they felt less stress.” The professor designed a study to test the effect of acupuncture on blood levels of the neuropeptide Y (NPY), which is secreted by the sympathetic nervous system in rodents and humans. This system is involved in the “flight or fight” response to acute stress.
Eshkevari gently conditioned the rats to become comfortable with the kind of stimulation used in electro-acupuncture – an acupuncture needle that delivers a small, painless electrical charge. This form of acupuncture is often used for pain management, she says, adding that she used electro-acupuncture to ensure that each rat would get the same treatment dose. She then selected a single acupuncture point to test on the leg below the knee, which is said to help relieve a variety of conditions including stress in humans.
The study used four groups of rats for a 14-day experiment:
Eshkevari and her research team found NPY levels in the experimental group came down almost to the level of the control group, while the rats that were stressed and not treated with acupuncture had high levels of the protein.
In a second experiment, she stopped the acupuncture in the experimental group but continued to stress the rats for an additional four days. The NPY levels remained low. “We were surprised to find what looks to be a protective effect against stress,” she says. The American Association of Nurse Anesthetists funded the research with a doctoral fellowship award to Eshkevari, and the National Institutes of Health’s National Center for Complementary and Alternative Medicine provided a grant for the study.
I’ve known Denise for a few years now and have received acupuncture treatment from her for lower back pain and stress. It gave me instant relief. Denise is great at what she does and has been a wonderful resource for me to have.
G.W.H., Portland, Or.
BLUE VALLEY ACUPUNCTURE serves the greater Walla Walla Valley area, Dayton and nearby towns of Waitsburg, Starbuck and Pomeroy in the southeast corner of Washington state.
Written by Shirley S. Wang
There’s growing acceptance that herbal medicines could be effective for medical conditions, but the scientific evidence to vault such a treatment into an approved drug is often lacking. As Shirley Wang explains on Lunch Break, researchers are making progress on a cancer treatment based on a

common herbal combination in Chinese medicine.
Scientists studying a four-herb combination discovered some 1,800 years ago by Chinese herbalists have found that the substance enhances the effectiveness of chemotherapy in patients with colon cancer.
Photo Researchers Inc.
Early studies show a traditional four-herb combination has cancer-treatment benefits. The herbs are Chinese peony (pictured), Chinese jujube, Chinese licorice and baikal skullcap.
The mixture, known in China as huang qin tang, has been shown in early trials to be effective at reducing some side effects of chemotherapy, including diarrhea, nausea and vomiting. The herbs also seem to bolster colon-cancer treatment: Tests on animals with tumors have shown that administering the herbs along with chemotherapy drugs restored intestinal cells faster than when chemo was used alone.
The herb combination, dubbed PHY906 by scientists, is a rare example of a plant-based product used in traditional folk medicine that could potentially jump the hurdle into mainstream American therapy. A scientific team led by Yung-Chi Cheng, an oncology researcher at Yale University, and funded in part by the National Cancer Institute, is planning to begin Phase II clinical trials to study PHY906’s effectiveness in people with colon cancer.

Many conventional medications are derived from individual chemical agents originally found in plants. In the case of huang qin tang, however, scientists so far have identified 62 active chemicals in the four-herb combination that apparently need to work together to be effective.
“What Dr. Cheng is doing is keeping [the herbal combination] as a complex entity and using that as an agent,” says Josephine Briggs, head of the federal National Center for Complementary and Alternative Medicine, which is helping fund some of the PHY906 research. “It’s polypharmacy,” or the equivalent of several drugs being administered at once.
Dr. Cheng began his research on huang qin tang about a dozen years ago when he sought a better way of dealing with the chemotherapy’s side effects. A variety of medications are currently used to treat these symptoms, but with varying success. A more effective technique could improve patients’ quality of life and possibly allow them to tolerate a larger dose of chemo, which might speed up their course of treatment, he says.
Dr. Cheng, who grew up in Taiwan, turned to Chinese traditional medicine, which often touts holistic treatments and multiple health claims for a single herb. In herbal literature he found mention of huang qin tang, a herbal combination traditionally used in China for gastrointestinal problems, and decided to test whether it could help cancer patients without compromising the effectiveness of the chemotherapy.

The research team began by giving mice with colon cancer high doses of irinotecan, a chemotherapy drug. Some of the mice also received varying doses of PHY906, the herbal combination. After four days, the animals that got the herbs seemed to experience fewer side effects. The herbs also appeared to improve the efficacy of the chemo, restoring damaged intestinal cells faster than with chemo alone and allowing the mice to tolerate doses of the drug that otherwise might have been lethal.
They followed with another experiment treating animals in four groups. One group received just the chemotherapy drug, another received just PHY906, a third group got both and the last group got nothing. The herb and drug combination worked the best at reducing side effects. As the researchers expected, PHY906 had no impact on the cancer when used by itself.
Further testing showed that PHY906’s effectiveness was diminished if any of the four herbs was eliminated, indicating that there is an apparent synergistic effect between them. This finding “got me serious about [PHY906],” says Dr. Cheng. The work was published in the journal Science and Translational Medicine in 2010. By submitting PHY906 to the scientific rigor of clinical trials, Dr. Cheng aims to win regulatory approval for the compound’s use in cancer treatment.
One challenge with using herbal medicines is that the ratio of the chemicals they contain isn’t consistent when plants are grown under different conditions. After testing various suppliers, Dr. Cheng ended up creating a biotechnology company sponsored by Yale called PhytoCeutica to carefully monitor growing conditions to ensure plants from different batches were pharmacologically consistent and to continue clinical development of the compound.

Why PHY906 works isn’t entirely clear, Dr. Cheng says. The herbal combination appears to have an anti-inflammatory effect on the gastrointestinal tract, according to work the group published in the journal BMC Medical Genomics last year. Dr. Cheng says he believes PHY906 works in at least three different ways in the body to control the side effects of chemotherapy, whereas conventional treatments work in just a single way.
So far, research data seem to support Dr. Cheng’s hunch about traditional medicine. “If it’s still in use after a thousand years there must be something right,” he says.
Write to Shirley S. Wang at shirley.wang@wsj.com
Bucking the Mainstream to Focus on Healing Herbs
Cancer researcher Dr. Yung-Chi Cheng -Yale University
When cancer researcher Yung-Chi Cheng set out some 12 years ago to study a traditional Chinese medicine, the initial reaction from colleagues and other experts in the field was “pretty bad,” he says.
Colleagues worried that Yale University’s Dr. Cheng, a mainstream, respected professor of pharmacology, was taking a professional risk by delving into possible herbal treatments for cancer. It wasn’t possible to get separate batches of herbs containing chemical compounds that were consistent, they told him. And there wasn’t evidence to support the claim that the herbs had any benefit. “It was rejectionist and narrow-minded,” Dr. Cheng says.
Nature’s Drugs
Some herbs and plants with possible cancer-treatment benefits.
Boswellia serrata (frankincense) Reduces inflammation
What it is being studied for: To reduce tumor growth and brain swelling in patients with gliomas
Nerium oleander (rose laurel)
Reduces inflammation and modulates the immune system
What it is being studied for: To use with chemotherapy drugs to treat advanced non-small-cell lung cancer
Valeriana officinalis (garden heliotrope)
Has sedating effects
What it is being studied for: To improve sleep in cancer patients undergoing treatment
Hypericum perforatum (St. John’s wort)
Has analgesic, sedative and anti-depressant effects
What it is being studied for: To reduce hot flashes in postmenopausal women with breast cancer
Source: National Cancer Institute
Born in Britain and raised in Taiwan, the 67-year-old Dr. Cheng mainly works at developing better cancer and antivirus compounds. He says he decided to move forward with the work on Chinese herbs on a part-time basis because he felt that whether the medical claims were true or not, they needed to be evaluated closely.
Over the years, the field’s view of this type of work has changed, says Dr. Cheng. With clinical evidence and data showing that the herbal product can be made to be consistent, he has experienced more acceptance from colleagues in the U.S. and internationally. In 2003, he started a global consortium of researchers and pharmaceutical companies studying traditional Chinese medicine.
Dr. Cheng, who earned his doctorate in biochemical pharmacology from Brown University in Rhode Island, has also found it easier over time to get published and to receive funding for the work with herbs, including as a potential treatment for the side effects induced by cancer chemotherapy.
Anticipating the skepticism he might face in developing a plant-based drug, Dr. Cheng didn’t publish his work in a journal until two years ago when he had consistent, clinical evidence and some understanding of the mechanism. “I might as well wait until the whole comprehensive story develops,” says Dr. Cheng. “Now I feel it’s about time.”
—Shirley S. Wang
Corrections & Amplifications
The common name of the plant Hypericum perforatum is St. John’s wort. In an earlier version of this article, a listing of herbs and plants with possible cancer-treatment benefits misspelled the name as St. John’s sort.

New Patient Spring Renewal Special! $20 off 1st Treatment
Denise Lane graduated from Oregon College of Oriental Medicine in Portland, Oregon, one of the top 3 schools in the country.
Denise provides gentle acupuncture in a calm and respectful environment to folks in Dayton, Waitsburg, Prescott, Pomeroy, Walla Walla and the corner of SE Washington area.
She utilizes not only Chinese TCM techniques but also a gentle Japanese style. Chinese herbs and other supplements are used. Specialties include shiatsu massage, cuppiing, guasha, electrical stimulation and trigger point therapy.
Denise treats many health issues including anxiety, asthma, allergies, fertility, back pain, shoulder pain, PMS. women’s health, TMD, Trigeminal neuralgia, stress, firbromyalgia, chronic fatiuge and more…..
Most insurance billed
sliding fee scale available